West Nile virus (WNV) is a neurotropic flavivirus meaning it has a strong preference for infecting cells of the nervous system. While most human infections remain asymptomatic or cause only mild illness, in some cases the virus crosses into the central nervous system (CNS), causing neuroinvasive disease such as meningitis, encephalitis, or acute flaccid paralysis. Neuroinvasion occurs in less than 1% of infections, but when it does, it can be life-threatening.
Routes of Neuroinvasion
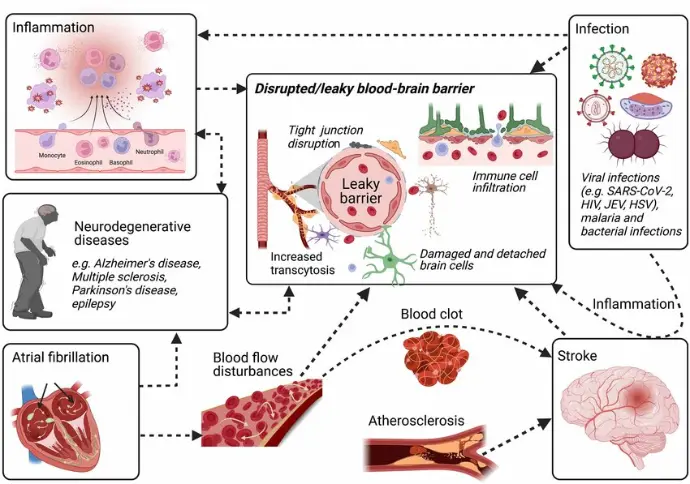
Blood–Brain Barrier (BBB) Disruption
Inflammatory Cytokines: Infection of peripheral tissues triggers systemic inflammation, leading to elevated TNF-α, IL-6, and matrix metalloproteinases (MMPs).
These molecules increase BBB permeability, allowing virus particles or infected immune cells to cross into the CNS.
The endothelial cells lining brain capillaries can also be directly infected, further weakening the barrier.
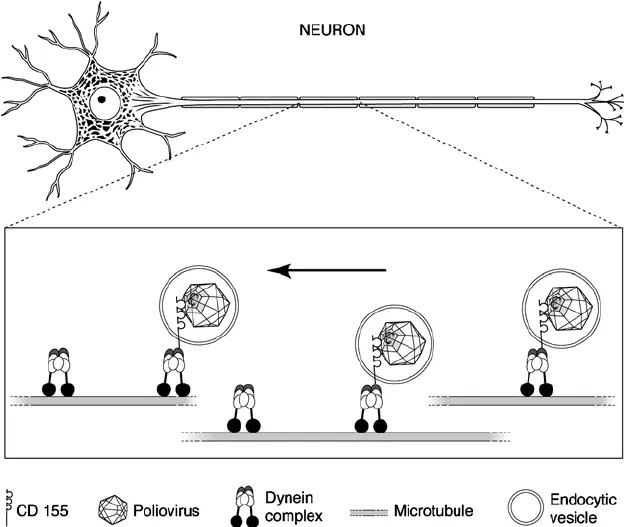
Retrograde Axonal Transport
- WNV infects peripheral neurons (e.g., in the skin, muscle, or dorsal root ganglia).
- The virus travels along the axons toward the spinal cord and brain using the cell’s own transport machinery.
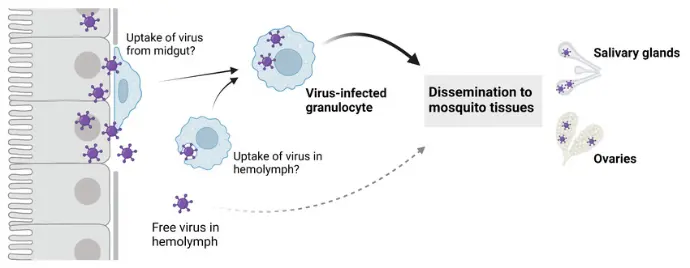
Choroid Plexus Entry
The choroid plexus, which produces cerebrospinal fluid (CSF), is less tightly sealed than other brain capillaries.
WNV may exploit this to enter the CSF and then spread into brain tissue.
Target Cells in the CNS

Neurons
Main Target especially in the brainstem, cerebellum, hippocampus, thalamus, and spinal cord.
Infection disrupts normal electrical signaling and triggers neuronal apoptosis.
Particularly vulnerable are motor neurons in the anterior horn of the spinal cord, explaining the acute flaccid paralysis seen in some patients.
Astrocytes
Can be infected but often act as viral reservoirs rather than rapidly dying.
They contribute to neuroinflammation by releasing cytokines and chemokines.

Microglia
The brain’s resident immune cells.
May be directly infected, but their stronger role is in producing inflammatory mediators that can damage surrounding neurons.
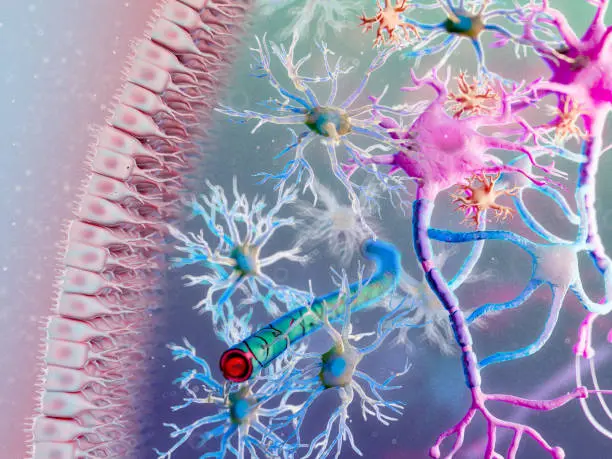
Oligodendrocytes
Occasionally infected; damage here can impair myelin maintenance and slow nerve conduction.
Pathological Consequences of Neuroinvasion
Encephalitis: Widespread neuronal infection and inflammation lead to confusion, seizures, and coma.
Meningitis: Infection of the meninges causes headache, neck stiffness, and photophobia.
Acute Flaccid Paralysis: Loss of motor neuron function in the spinal cord results in limb weakness or respiratory muscle paralysis.
Long-Term Sequelae: Survivors may experience persistent neurological deficits, fatigue, or memory problems.
Host–Virus Interaction in the CNS
Immune Control: Once WNV is inside the CNS, immune cells such as T lymphocytes are critical for clearing the infection.
Collateral Damage: Unfortunately, the same immune response that helps clear the virus can cause bystander neuronal death.
Persistence: In some animal studies, WNV RNA persists in the CNS for weeks to months, suggesting the potential for chronic inflammation.